New research has suggested that contracting COVID-19 increases the risk of an Alzheimer’s diagnosis for senior individuals. The study, which came out of the medical community in Cleveland, analysed the health records of millions of Americans aged 65 and over.
Dr. Pamela B. Davis was one of the lead scientists working on the study, which was published in the Journal of Alzheimer’s Disease in September.
She noted that prior infections and inflammation were two key factors in the development of Alzheimer’s. “Since infection with SARS-CoV2 has been associated with central nervous system abnormalities including inflammation,” she said, “we wanted to test whether, even in the short term, COVID could lead to increased diagnoses.”
The study looked at the electronic health records of 6.2 million American seniors, divided into those who had had COVID (410,), and those who hadn’t (5…). Researchers also looked at outcomes based on age, sex, and race, to see whether demographic factors affected the relationship between COVID and Alzheimer’s.
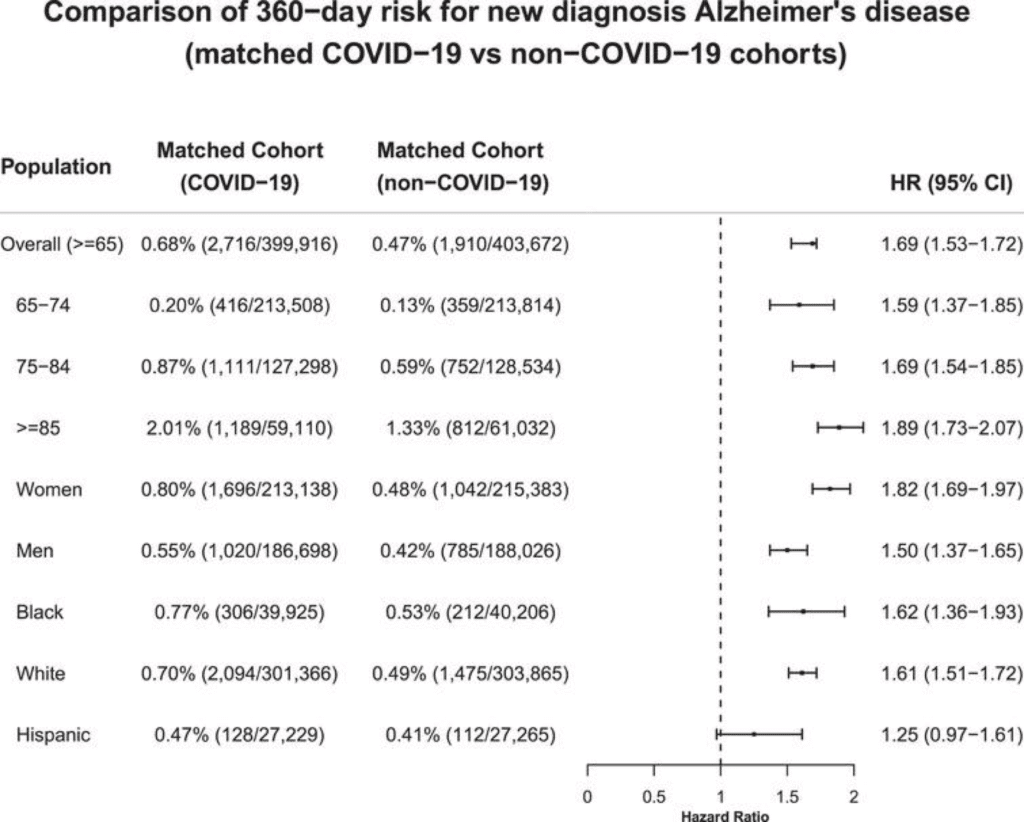
Overall, they found that contracting COVID seriously increased an older individual’s chances of developing Alzheimer’s Disease. The risk in the COVID cohort was 0.68%, compared to 0.47% in the matched non-COVID group. It was even higher for those over 85 years old, and for women.
The study does not conclusively tell us whether COVID directly triggers Alzheimer’s or simply accelerates it; but the ‘bidirectional relationship’ between the two conditions is undeniable.
“If this increase in new diagnoses of Alzheimer’s disease is sustained,” noted Davis, “the wave of patients with a disease currently without a cure will be substantial, and could further strain our long-term care resources.”
COVID and Cognitive Decline
The findings of Davis and her colleagues support numerous other studies reporting the neurological consequences COVID can have.
In some cases, COVID infection has directly affected the brain, where patients have suffered encephalitis, thrombotic incidents, and brain invasion. The widely-reported loss of smell and taste is another clear indicator of cognitive damage.
A 2020 study out of Wuhan found incidence of cognitive impairment among patients aged 60+ was higher in COVID survivors. When tested for cognitive decline 12 months after being discharged, 12.45% of COVID patients showed signs of impairment.
Much of Davis’ team on this most recent Alzheimer’s study also joined her on an earlier report, which found patients suffering from dementia were twice as likely to get COVID. Said study reported that 6-month mortality and hospitalisation risks in patients with dementia and COVID were 20.99% and 59.26%, respectively. The dementia study looked at the health records of almost 62 million people.
Key risk factors for dementias include cardiovascular diseases, diabetes, and obesity. Many of these very conditions are also comorbidities for poor treatment outcomes for COVID. Davis’ group has also pointed out that cognitive impairment due to dementias can prevent patients from advocating for and receiving appropriate and timely COVID care.
Approximately 50 million people worldwide suffer from Alzheimer’s and other dementias. “The long-term consequences of COVID are still emerging,” comments Davis. “It is important to continue to monitor the impact of this disease on future disability.”
Cover photo by Robina Weermeijer on Unsplash.
Follow Maddie’s journalism on Twitter.
Sign Up To Our Free Newsletter