Reports have previously suggested there was a bump in prescription mental health drug use during the COVID pandemic and lock-downs. ADHD drugs even saw worldwide shortages in 2023.
How substantial and lasting was the effect of COVID on psychiatric drug use? The NSW Ministry of Health recorded a 19.2% increase in SSRI prescriptions per annum since the beginning of the pandemic.
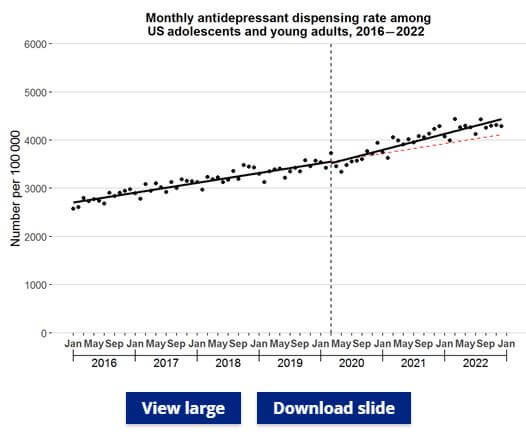
Now, a full review of antidepressant prescriptions in the US, published at the end of February by the journal of the American Academy of Pediatrics, shows a startling increase in the six years from 2016.
Between January 2016 and December 2022, there was a 66% increase in antidepressant prescriptions. On the back of steady yearly increases before the pandemic, antidepressant prescription increased 63% faster from the start of the pandemic onwards.
The most shocking figure relates to antidepressant prescription to girls. An increase of 130% over the rate of pre-COVID prescription was recorded for girls aged 12 to 17.
A higher proportion of women than men use SSRI antidepressant drugs. But that moderate disparity is far from accounting for the increase shown by this research in prescriptions of these mental-health drugs to girls.
For some reason, the pandemic and lock-downs had a much harsher impacts on the mental health of girls than on young women or males. The study authors noted that since the start of the pandemic, suicide attempts among adolescent girls increased 50%, compared to a 3.7% increase among adolescent males and a 5.8% increase among young female adults (i.e. 18 to 25 years old).
In contrast, new antidepressant prescriptions actually slowed for adolescent males and young men in the US northeast and midwest from COVID onward.
NZ-based qualitative researchers found young women often feel “not fully myself” while taking antidepressants. However, they also found a depression diagnosis and antidepressant prescription gave a sense of legitimacy to pre-existing distress.
Thumbnail image courtesy of @daniloalvesd via Unsplash.