Recently-released data from the NSW Department of Health shows tens of thousands of people have battled COVID reinfection. Omicron sub-variants are wreaking havoc on vaccine-induced immunity, but anecdotally, having COVID gets easier each time, right?
A new study from the US suggests not.
Reinfection Runs Rampant
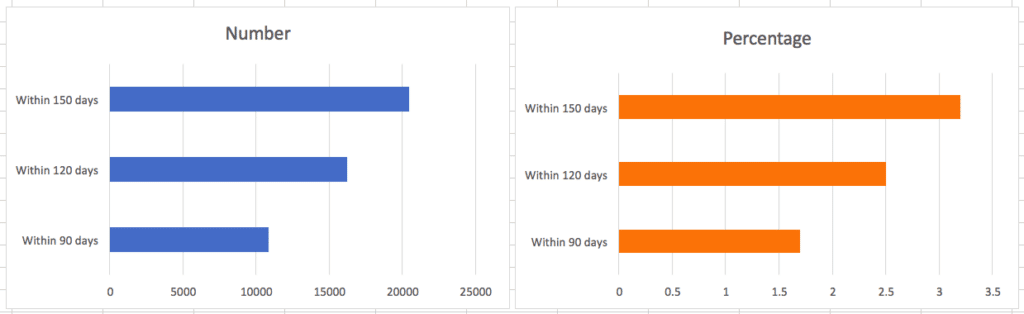
NSW Health has released analysis of data from 639,430 who caught COVID for the first time in January – towards the start of the Omicron wave. Their findings showed that within 5 months, over 20,000 people had been reinfected.
Just last month, the Australian Health Protection Principal Committee announced that the COVID reinfection period was being reduced from 12 weeks to just 28 days. The reinfection period refers to the time after first infection when risk of reinfection is lower, due to natural immunity.
Luckily, of the thousands of Aussies for the second, or third (or 4th, or n-th) time, most report milder illness. Experts like Nick Wood, a paediatrician and immunology specialist at USYD, hope that over time, people are better able to cope with new variants because of past infections and vaccines.
Wood’s vision for the future is “that if you do get sick, you get sicker for less time, and you have less of the virus, so you shed less. Hopefully, this will just go the way of being diluted to the effect that it becomes more like a common cold.”
US Study: Reinfection Raises Risks
Unfortunately, a recent study by scientists from Washington University School of Medicine and VA Saint Louis Health Care System is throwing a shadow over such hopes.
The study looked at a huge sample size of over 5 million Americans, drawing on databases from the US Department of Veterans Affairs. The results showed that, compared to participants with first-time infection, those with reinfection exhibited heightened risk of all-cause mortality, hospitalisation, and having at least one post-COVID condition.
Risk calculations were set out in terms of excess burden per 1000 persons at the 6-month mark. Reinfected people showed an excess burden of all-cause mortality estimated at 23.8 per 1000 persons at 6 months, for example.
Vaccination had no significant bearing on results, with risks of mortality, hospitalisation, and further illness evident across unvaccinated participants, as well as those with one, two, or more doses.
Furthermore, the study showed that risk and excess burden increased in line with the number of infections. For example, compared to the non-infected control group, people with one infection were at greater risk of at least one post-COVID condition – with a burden of just over 84.
But for those who had two infections, the risk rose dramatically, with a burden of 234.58. And it was highest in participants with three or more infections – a burden of 362.82. Similar results were recorded for mortality and hospitalisation.
The study’s findings complement emerging science showing that your risk of contracting Long COVID also increases with subsequent infections.
Clearly, reinfection is not to be taken lightly. As the authors of this study conclude, “even combined natural immunity (from prior infection) and vaccine-induced immunity does not abrogate risk of adverse health effects following reinfection.”
COVID isn’t going away any time soon. And in the long-term, both individuals and governments would do well to actively avoid reinfection as much as possible.
Cover photo by Fusion Medical Animation on Unsplash
Follow Maddie’s journalism on Twitter.
Sign Up To Our Free Newsletter